Overview
In laparoscopic urologic surgery, urological problems are fixed without the patient experiencing a lot of pain. It is a minimally invasive procedure that uses a laparoscope, which includes a built-in camera, together with a number of long, thin surgical tools. Small incisions are used to put it into the body. Patients who have this procedure benefit from substantially better post-operative pain management, a shorter hospital stay, a rapid recovery period, and improved outcomes.
Nowadays, laparoscopic urologic procedures use robotic technology. The surgeon’s vision and dexterity are much improved during robotic surgery. Particularly in radical prostatectomy for prostate cancer, robotic technology has become more and more prevalent.
What Situations Call for Laparoscopic Urologic Surgery?
The use of laparoscopic urologic surgery is used to treat a wide variety of benign and malignant urologic disorders. Laparoscopic surgery is most frequently used for pyeloplasty, nephrectomy, partial nephrectomy, radical prostatectomy, and radical cystectomy.
Laparoscopic urologic surgery preparation
The relevance of standardized imaging techniques cannot be overstated. The outcomes of specific preoperative imaging tests heavily influence the decision for the majority of surgical procedures. The size of the damaged organs can occasionally make laparoscopic surgery difficult. For instance, the space needed for specimen mobilization is constrained if renal tumors in the kidneys are particularly large. The operative space is also reduced if a nearby organ is pathologically enlarged, thereby limiting the ability of a surgeon to undertake laparoscopic surgery.
The doctor has a duty to explain to the patient any potential surgical risks associated with laparoscopic urological operations. The patient should be aware that some problems, such as fibrosis or adhesions, cannot be treated using laparoscopic surgery, and the doctor may have to perform an open procedure instead.
Although the laparoscopic method results in relatively less blood loss, the surgeon nevertheless makes sure that packed red blood cells are on hand before the procedure, wherever anticipated.
Surgery in urology: Process
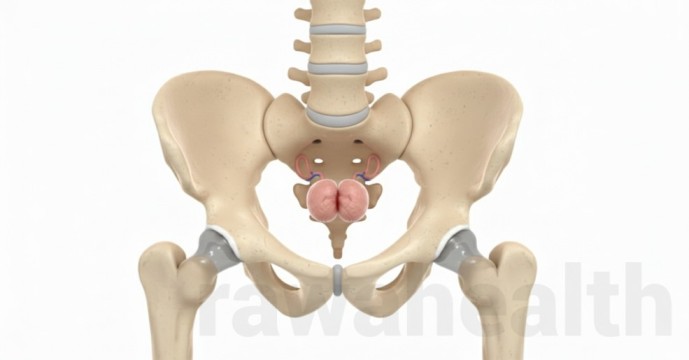
Positioning the patient
The location of the patient is determined by the surgical technique chosen. Any dissection of the adrenal or renal glands is performed via a transperitoneal route. In this method, the patient is positioned in a modified lateral position that makes the abdominal cavity easily accessible. The patient is positioned rigidly to the side when using a retroperitoneoscopic technique. The surgeon alone determines whether to use a transperitoneal or retroperitoneal technique. Trendelenburg is a particular posture used during pelvic procedures like prostatectomy, when the head is lowered and the leg is lifted.
Technical Methodology
- Transperitoneal Technique A laparoscopic procedure begins with the establishment of a pneumoperitoneum. Gas in the peritoneal cavity is referred to as pneumoperitoneum. In laparoscopy, CO2 is typically utilized for insufflation. Pneumoperitoneum is achieved using the open method and the Verress needle. The needle is placed using the Verress technique near the umbilicus’ cranial edge. To prevent any harm to the bowels or any significant blood arteries, extra care must be exercised. The open strategy is used to steer clear of any potential Verress technique problems. A significantly larger incision is made for the surgery when using an open method. Since the same incision can be utilized for post implantation and/or specimen retrieval, the size of the incision is not very significant.
- Extraperitoneal technique: In contrast to intraperitoneal technique, adequate space is not accessible in extraperitoneal approach; as a result, space must be produced artificially. A minor incision is made in the mid-axillary line at the 12th rib, and the majority of the procedure is a balloon dilatation to create space for the surgery. The psoas muscle and the Gerota’s fascia’s posterior layer form the working space. Trocar introduction requires a sufficient workspace.
- Placement of Ports: During surgery, ports serve as a doorway for the insertion of additional tools. Only when the workspace has been formed are the ports secure. After the laparoscope has been inserted, the operating room is thoroughly examined for adhesions and other anomalies. Under the surgeon’s direct supervision, more Ports are added. To prevent harm to the sutures, extra care is necessary when inserting the Port into the cavity.
Nephrectomy Surgery
Two things are kept in mind before the surgery, one is excellent visualization, and the other one is the duplication of open surgery principles. Similar to an open surgery, laparoscopic devices are composed of scissors, dissectors, vascular staplers, graspers, scalpels and more. The only difference is that they are simply elongated. Whenever, laparoscopic procedures require specimen retrieval, it is achieved using a specimen retrieval bag. It is inserted through the port and then unfolded in the surgical space.
The specimen is entrapped in the bag, and then it is closed for extraction. Once the specimen is extracted, the laparoscope is re-introduced to verify the presence of bleeding. In order to control any sort of unexpected bleeding, the ports are removed under direct vision. The pneumoperitoneum is deflated before the removal of the last trocar. These small incisions are then closed similarly as performed in an open surgery.
Complications After Urology Surgery
What Are the Advantages of Urology Surgery?
The most significant advantages of laparoscopic urology surgery procedure include:
- Reduced Bleeding: This reduces the chances of requiring a blood transfusion.
- Smaller Incision: This not only reduces pain but also shortens recovery time, resulting in less post-surgery scarring and surgery marks.
- Less Pain: Because it is a minimally invasive surgery, patients experience minimal pain.
- Less Hospital Stay: Although the surgery time is usually slightly longer, the hospital stay is comparatively less in this surgery. In many cases, the patient is discharged the same day.
- Reduced Risk of Catching Infections: The surgery decreases the exposure of internal organs to external contaminants thereby reducing the risk of catching infections.